— What made you think he was not really a doctor?
— I could read his handwriting!
All joking aside, illegible scrawls can result in serious and even fatal errors. Together with multiple other prescribing mistakes, they are a component in five to nine percent of medical orders, creating significant risks for patients.
The situation can be remedied with wider adoption of electronic prescribing (eRx) and test ordering technologies. This article discusses software that eliminates paperwork. It also provides ways to address different challenges the technology poses.
What is CPOE and how is it used in healthcare?
CPOE stands for computerized provider or physician order entry. This technology enables doctors to order drugs, tests, consultations, and other medical products and services electronically instead of writing prescriptions by hand.
The first CPOE system was built in 1971 by NASA Space Center and Lockheed Corporation for a hospital in California. Similar to other early solutions developed in the 1970-1980s, it featured only basic functions while costing hundreds of millions of dollars. Besides, innovations met resistance from staff.
It was not until the late 1990s that CPOE started to bring real value to hospitals due to technological advances, decreased cost of development, and enhanced computer literacy of medical professionals.
CPOE major integrations and workflow
Modern CPOE systems come as an important part of the healthcare IT infrastructure. Usually, they extend the functionality of EHR (Electronic Health Record) systems and employ a clinical decision support module to check drug-drug and drug-allergy interactions, verify the dosage, and prevent duplicate therapy.
A CPOE solution can be also pre-integrated with a medical practice management platform to flag orders that require preapproval from an insurance plan. This practice helps hospitals minimize the number of denied claims.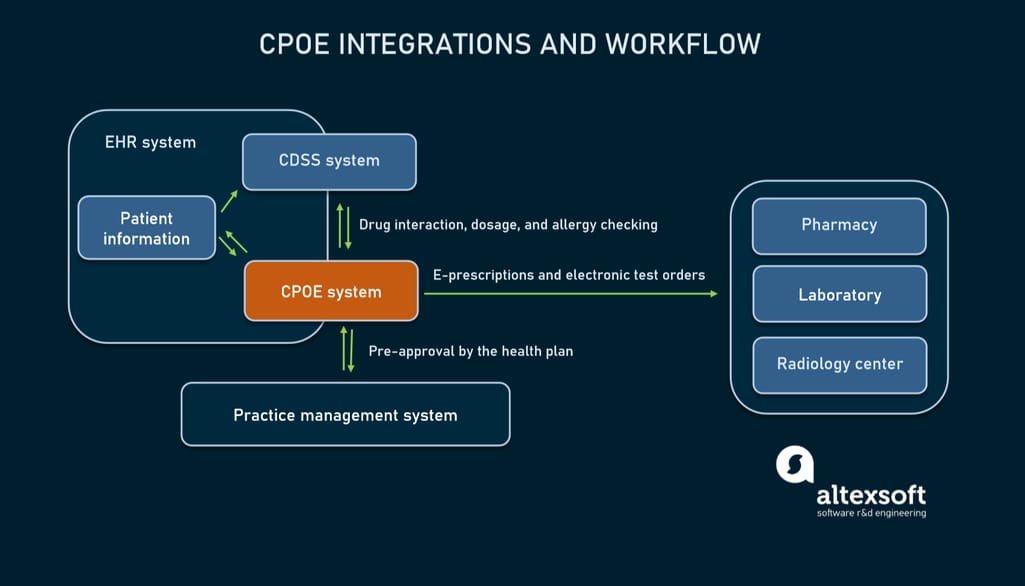
How a CPOE system fits into healthcare IT infrastructure.
In the common scenario, the workflow involving CPOE looks as follows.
1. A user (physician) logs in to an EHR system.
2. The EHR system confirms that the user is authorized and initiates the ordering process via the CPOE system.
3. The physician creates or modifies an order for medications, laboratory, or radiology tests.
4. The order is validated against a patient’s medical history, a knowledge base of a clinical decision support system, and a health insurance plan stored in a practice management system.
6. After all the checks, the order is sent to a product or service provider’s system (a pharmacy, laboratory, etc.).
7. The order becomes part of the patient’s record in the EHR system.
These steps make prescriptions transparent and trackable, less prone to error and fraud. The next section will dig deeper into the advantages of CPOE.
CPOE benefits
E-prescribing and electronic test ordering drive a lot of improvements in terms of efficiency and patient safety. The most widely mentioned benefits of using CPOE are
- elimination of lost orders;
- avoidance of ambiguities caused by illegible handwriting;
- prevention of medication errors. According to the Leapfrog hospital survey, so-called adverse drug events contribute to 7,000 deaths annually. A CPOE module paired with a clinical decision support component can reduce medication error rates by 55 to 88 percent;
- reduced costs on long-term healthcare. The same survey shows that after implementation of CPOE, the length of a hospital stay reduced by 0.9 days with expenses falling 13 percent;
- better reimbursement rates thanks to automatically alerting to orders that require pre-approval from insurance companies;
- transparency of ordering processes; and
- improved administration. The system ensures that pharmacies and laboratories get orders faster. At the same time, medications and services are received by the right person at the right time in the correct dosage or order.
All these benefits are not only desirable for hospitals, they are becoming mandatory across the USA — with the arrival of new regulations.
CPOE Meaningful Use and EPCS compliance
The adoption of electronic prescribing software across the US was spurred on by the Meaningful Use program, later renamed the Promoting Interoperability (PI) program.
According to PI requirements, hospitals must record over 60 percent of medication, laboratory and radiology orders using CPOE. Besides that, over 60 percent of all permissible prescriptions must be automatically checked against a drug formulary (an assortment of medications managed by a health insurance plan) and transmitted to pharmacies electronically.
Another law speeding up the implementation of eRx technologies is SUPPORT for Patients and Communities Act aimed at fighting opioid addiction and misuse. Starting in January 2021, it obligates healthcare organizations to use electronic prescribing of controlled substances (EPCS).
Some states take things a step further: For example, in California, it will be compulsory to make all prescriptions electronically — in accordance with the new legislation effective January 1, 2022.
New laws don’t bring large changes to the traditional e-prescribing workflow mentioned above. At the same time, to be EPCS-compliant, CPOE systems must meet a few key requirements of the Drug Enforcement Agency (DEA).
Two-factor authentication (2FA). The system can utilize two of the following options:
- a password or response to a private question,
- a biometric identifier (fingerprint or iris scan),
- a PKI (public key infrastructure) smartcards,
- an OTP (one-time-password) token generated by an application, or
- a hard token.
Two-step control. Two people must authorize each prescription for controlled drugs. The first confirms that a physician is entitled to sign the prescription. The physician, in turn, verifies his or her identity via the two-factor authentication process.
Integration with the state PDMP database. On the pharmacy side, when dispensing controlled drugs to patients, chemists must add the order to the Prescription Drug Monitoring Program (PDMP) — a network of independent electronic databases created to track prescriptions of controlled substances within each state.
E-prescribing and CPOE systems vendors
Many modern EHR systems have a prebuilt CPOE or e-prescribing module. But the original component may be inefficient, incomplete, or noncompliant with new regulations. In this case, you can use a third-party, off-the-shelf solution available on the market. Here are some offerings from popular CPOE and eRx system vendors.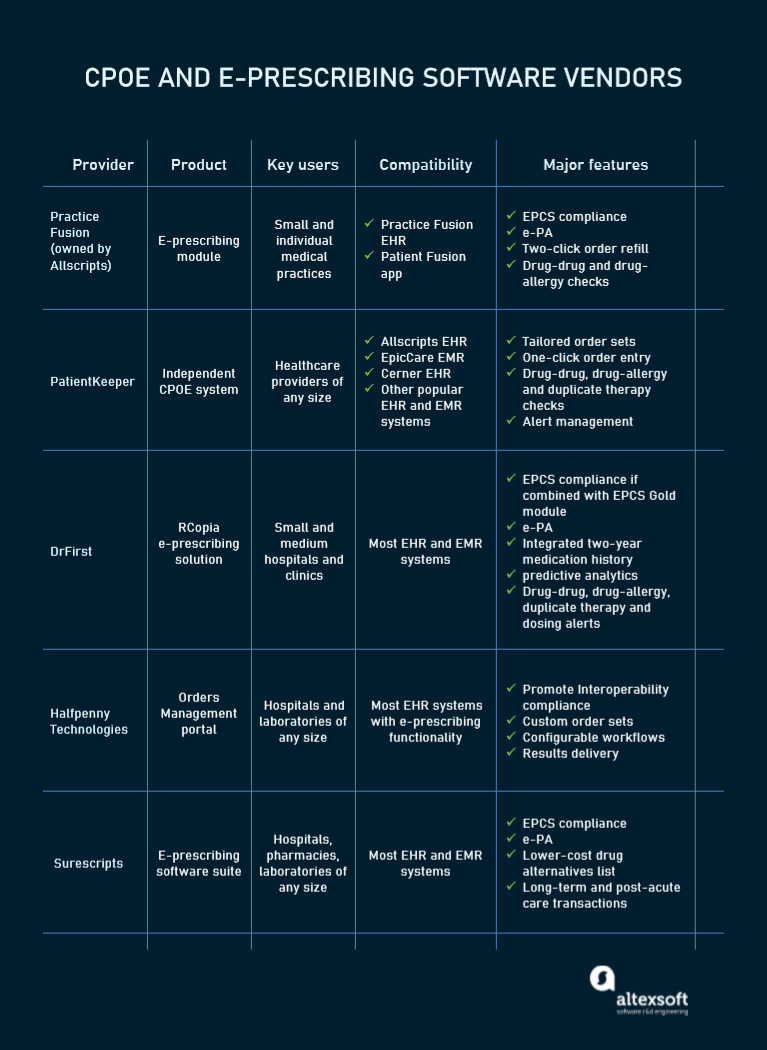
A brief comparison of electronic ordering solutions.
Practice Fusion: the best solution for solo practitioners
Practice Fusion, the number one EHR provider for solo and small practices, is owned by the healthcare IT giant Allscripts Healthcare Solutions. Its CPOE package extends the company’s core system enabling physicians to send e-prescriptions to over 98,000 national pharmacies. The module speeds up the ordering process with
- electronic prior authorization (e-PA), a feature ensuring the safe and appropriate use of selected drugs and medical procedures,
- prefilled SIGs (standard parts of prescriptions describing how to use the medicine);
- two-click prescription refills;
- prescribing multiple medications in one order; and
- automated drug-drug and drug-allergy checks.
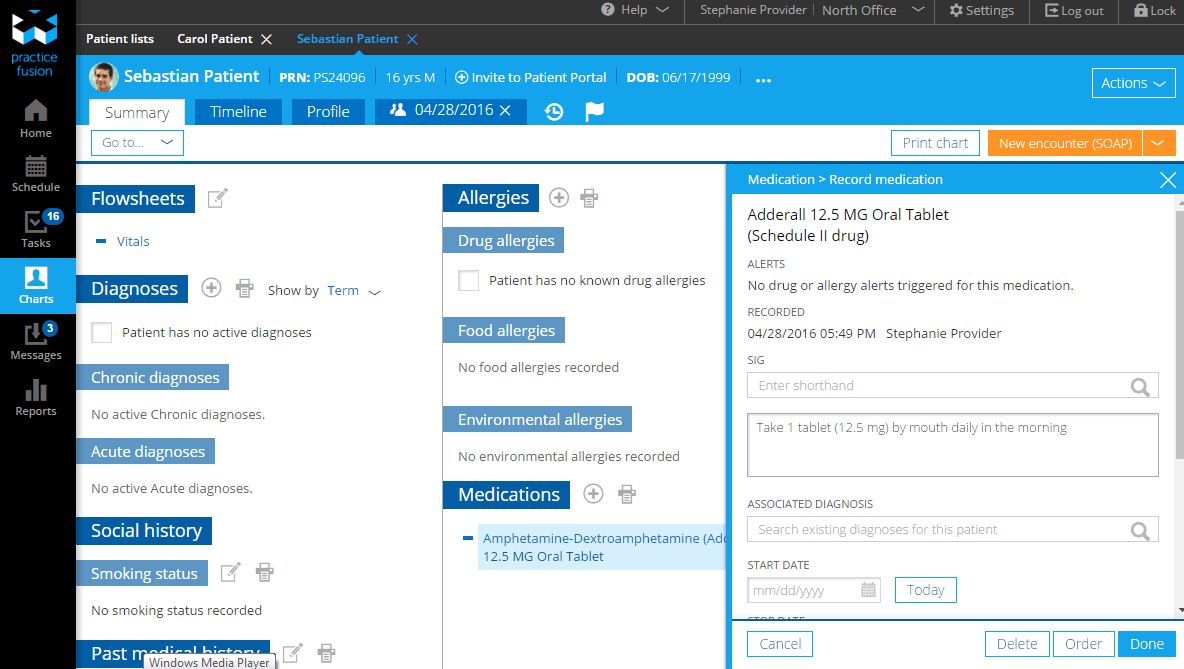
Checking medications against drug, food and environmental allergies mentioned in a patient’s health record.
Teamed with cloud-based app Patient Fusion, the system connects physicians with their patients for clarification of specific questions, sends reminders, and gives patients access to information regarding their drugs and tests.
PatientKeeper: a vendor-agnostic module to complete the current infrastructure
A web-based and mobile CPOE solution from PatientKeeper integrates with widely-used hospital EHR and EMR systems including EpicCare, Allscripts, Cerner, and others. It enables physicians to enter orders from a smartphone, tablet, or PC and streamlines the end-to-end CPOE process supporting
- order sets tailored to individual physician workflow;
- one-click entry of pre-defined “favorite” orders;
- drug-drug, drug-allergy, and duplicate therapy checks; and
- alert management to distinguish and send only critical notifications.
Rather than replace a working IT infrastructure, PatientKeeper CPOE is designed to fit into any workflow, saving hospitals time and money. Today, the software is used by over 400 healthcare providers and 70,000 physicians across the US, Canada, and UK.
DrFirst: e-prescription with analytics capabilities
DrFirst offers an e-prescribing system called Rcopia with an embedded decision support element that generates drug-drug, drug-allergy, dosing, and duplicate therapy alerts. It also features
- medication history data feed enabling physicians to instantly view information on drugs taken by a patient for the previous two years;
- electronic prior authorization; and
- predictive analytics capabilities, which mean that Rcopia can analyze e-prescribing patterns to make medication decisions faster and with fewer clicks.
For compliance with the EPCS rules, you need to combine RCopia with EPCS Gold — a separate software module, which is currently integrated with over 250 EMR, EHR, and other healthcare information systems.
Halfpenny Technologies: electronic test orders for Promoting Interoperability compliance
The company’s Orders Management portal streamlines processes of entering orders. It routes them to laboratories, allowing doctors to schedule and reschedule laboratory tests in one click. Once ready, test results are returned electronically for further reviewing.
The solution easily integrates with disparate EHR systems that already have e-prescribing modules but are not equipped with test-ordering functionality to meet Promoting Interoperability standards.
Surescripts: medication management with focus on long-term care
Surescripts provides a software suite for medication management. Its core e-prescribing application enables physicians to perform standard transactions, namely creating, refilling, changing, and canceling a prescription request.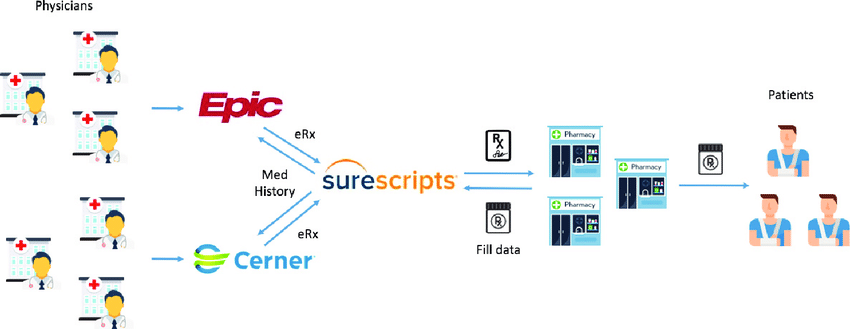
E-prescription process with Surescripts software. Source: A Decentralized Blockchain Ledger for the Management of Medication Histories
The main module can be combined with separate components to add the following capabilities:
- electronic prior authorization,
- compliance with EPCS standards,
- access to eligibility and formulary information to find drug and channel alternatives, and
- transactions specific to the long-term and post-acute care.
Surescripts solutions integrate with different technologies and workflows, connecting customers and end users into the Superscript Network Alliance. This includes pharmacies, EHR technology vendors, hospitals, care providers, and other players.
CPOE challenges to adoption and ways to alleviate them
Besides dividends, CPOE entails a range of adoption problems. Typically, health organizations face the following obstacles to technology implementation.
Integration complexity
Even off-the-shelf solutions can’t be introduced into the workflow fast: They require a massive amount of costly customization for each hospital, clinic, laboratory, or other healthcare provider. Things become even more complicated when the organization uses software from different vendors.
Best practices. If possible, stick to the same provider or, at least, contact your EHR vendor to make sure that the new solution is compatible with your existing platform. Another option is to create a custom solution that will fit your needs more accurately. Though custom development takes time, in most cases, the efforts are generously repaid in the future.
Process gaps
Unfortunately, technologies that work fine on paper are not always perfect in practice. Implementing new software often disrupts the habitual workflow and may cause such problems as a drop in productivity, complaints from employees or even errors posing risks to patients. The speed of adoption depends on prior experience of personnel, the number of new features to master, and other factors.
Best practices. Some hospitals deliberately slow down software implementation giving employees time to get accustomed to the new routine. They introduce features one by one minimizing resistance to change from physicians and preventing reductions in productivity. Another benefit of this approach is the ability to thoroughly test each feature and identify software bugs during the training period.
Updating and maintenance concerns
The healthcare company should maintain and update its e-prescribing software to align it with changes in the industry, new business requirements, and actual clinical guidelines. Without timely support and upgrade, the CPOE system may become obsolete.
Best practices. As a general rule, CPOE order sets must be reviewed every 6 months to ensure their relevance. Before choosing a system, it makes sense to learn about the availability and level of technical support your vendor provides after implementation. If it’s not sufficient, you need to look for an external company that will deliver systematic updates and maintenance services and make recommendations for improvement.
Introducing new errors
Unfortunately, while eliminating some types of errors, CPOE systems may introduce new ones. For example, an auto-complete function increases the risk of overlooking the right drug and selecting the wrong one.
Best practices. It’s highly recommended that hospitals regularly test their software to estimate the percentage of medication ordering errors, spot the sources of problems, and take measures to prevent them. Such testing is performed by the Leapfrog Group, a nonprofit organization that aims at enhancing the safety of American healthcare. Toward this goal, they annually check CPOE systems at hospitals against the Group’s standards. 2020 became an exception, though: The organization called off CPOE evaluation because of the COVID outbreak, with a promise to bring it back in 2021.
Meanwhile, pandemic or not, you need to redouble attention to electronic ordering processes. Ongoing monitoring of defects, finetuning of system settings, and additional checking of final orders by a practitioner are essential to avoid or at least minimize adverse effects and financial losses. CPOE is only a useful tool, not a panacea to all issues around prescribing.

