Today, over 90 percent of hospitals provide patients with a platform to view, download, and transmit their health information. Cool, right? Well… Only 30 percent of patients end up using it. Most people simply don’t see the need to open the portal that hosts lab reports they’ve already downloaded to their computer.
Technology is underused. Many clinics adopted a patient portal back in 2014 to receive payment under the EHR Incentive Programs. Healthcare providers rushed to incorporate patient engagement features just to pass the minimum 5 percent usage rate. This resulted in clunky platforms with limited features that clinics don’t see the need to improve.
So, let's dig into the ins and outs of building a portal that patients will love using -- and how that will benefit providers as well.
What is a patient portal and its benefits?
A patient portal or a personal health record (PHR) is a secure application that allows patients to access their personal health information (PHI). That’s a short version of a definition. Additionally, a portal has the potential to be a place for addressing all types of healthcare needs, being limited only by the capabilities of your application. This includes
- billing and payment,
- text message communication,
- medication management,
- appointment booking,
- educational materials.
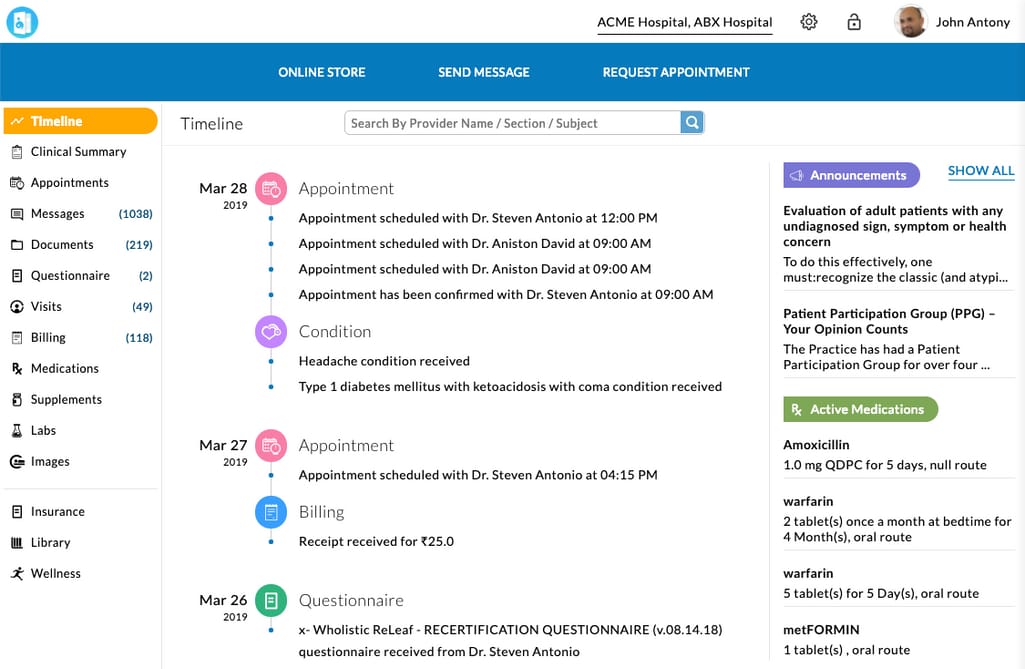 An example of a patient portal that offers a variety of capabilities Source: ChARM Health
An example of a patient portal that offers a variety of capabilities Source: ChARM Health
Why does patient engagement matter? Basically, because no quality of care, no effort, no technology advancements make sense if a patient fails to take their meds, doesn’t follow a treatment procedure, or simply avoids making an appointment. Patient engagement is about meeting people halfway and giving them resources to support themselves. The best resource for that is a patient portal. And it can benefit not only patients, but a hospital as well. Here are some advantages of patient portals for clinics.
Automating clinical admin tasks. Serving as an extra communication tool between your clinic and patients, it eases the staff workflow. Appointment scheduling, sending notifications and reminders, data collection and organization can be done in the background and without human errors.
Streamlining telemedicine offerings. Telehealth solutions have been in great demand since the start of the pandemic and they will keep growing as more clinics implement them. Although there are independent telehealth provider programs, many of those features can be and are integrated into patient portals.
Delivering competitive service and higher level of care. The availability of a feature-rich portal attracts patients who appreciate the convenience.
Implementation options and why you should build a custom portal
Now, there are three options for portal implementation. If you have a portal, it’s likely that it’s been acquired via the first method. Let’s review and compare them.
Acquire a portal from your EHR provider
Many certified EHRs like eClinicalWorks, Allscripts, Athena Health and Cerner offer patient-facing products already integrated with your EHRs for an extra fee.
Pros: These products are neatly intertwined with your system and can be easily implemented and understood by your hospital staff. If you have one of major EHRs, you likely have their portal as well. This method doesn’t come without drawbacks, though.
Cons: First, when picking the first available option, you don’t explore the wide range of opportunities on the market. Second, if your staff already hates their EHR, they won’t be a big advocate for the portal either. And all problems from one system will migrate to the other one.
The second scenario can save you from these problems.
Buy a separate patient portal solution
Solutions for many patient portal functions can be acquired separately, from third-party providers.
Pros: Dedicated patient portals usually deliver a more engaging experience and advanced features. Or you can even mix and match different solutions depending on your current needs and capabilities. For example, opt for a smart scheduling tool, a HIPAA compliant application for billing, and a reminder system.
Cons: This will require some effort on your part as you will need to seamlessly integrate those disparate products with your EHR and each other and train physicians and patients to use them. Although you will have more choice over the tools you acquire, you will have to compromise as well. And some things like usability, limited functionality, or simply a bad fit for your customer base might prove a product completely ineffective.
So, let’s talk about the option that might cover these drawbacks.
Build a custom patient portal
Here, a provider teams up with a healthcare technology partner on the design and development of a portal. There are many reasons why businesses choose to develop custom applications.
Pros: You will have full control over functionality, usability, and the choice of technologies. This will allow you to create a tool specific to your clinic’s workflow, patients, and the IT ecosystem. You will also be able to take into account unsuccessful examples of patient portals and address their problems in your application.
Cons: Custom applications come with a higher budget and long development time.
In this article, we want to focus on the third option since this is the only way you can influence the inner workings of the portal and improve the poor adoption rate. But if you plan to acquire a finished solution, it will be a great guide for you to learn what to look for.
Challenges of building a patient portal
There are three main foundations to consider when building a patient portal:
- Patient engagement. This is the core task that ensures that patients find value in the tool and know how to use it.
- Physician engagement. Clinicians, traumatized by numerous problems with EHRs, fear that using a portal will increase their workload. And here are other reasons for their repulsion, which we will cover further.
- Security and interoperability. It’s critical to achieve seamless data exchange between a portal and an EHR. At the same time, a portal adds to an always-present concern of data breaches in the healthcare domain.
We’ll give practical recommendations for managing all these concerns. But let’s start with the largest one -- catering to patients.
How to engage patient portal users
Why are current portals not engaging? There are three reasons.
Limited functionality. Studies show that many (37 percent of respondents) often don’t see how using a portal can improve existing care. “If you ask an otherwise healthy individual, ‘Why would you use the portal?’ they would just look at you with a blank stare and say, ‘There's nothing there,’” said Thomas Selva, MD, from the University of Missouri Health Care.
Poor usability. The flawed usability of health IT is the topic of many anecdotes and a source of many frustrations. When people can’t succeed at fulfilling the simplest tasks like navigating to the needed function, they get discouraged to try again.
Lack of training and encouragement. Multiple studies show that only a small part of the population benefit from patient portals. Patients who are young, female, married, with higher income, and a history of hospitalizations are the most active portal users. In a different study, the same group of people were the ones who utilize patient-provider messaging features the most, while non-millennial, non-white participants living in low socioeconomic neighborhoods were likely to not exchange messages at all.
Let’s start by drafting the list of features that can be useful to the widest user base.
Implement a wide set of patient portal features
Here are some features that surveys participants displayed the most enthusiasm about.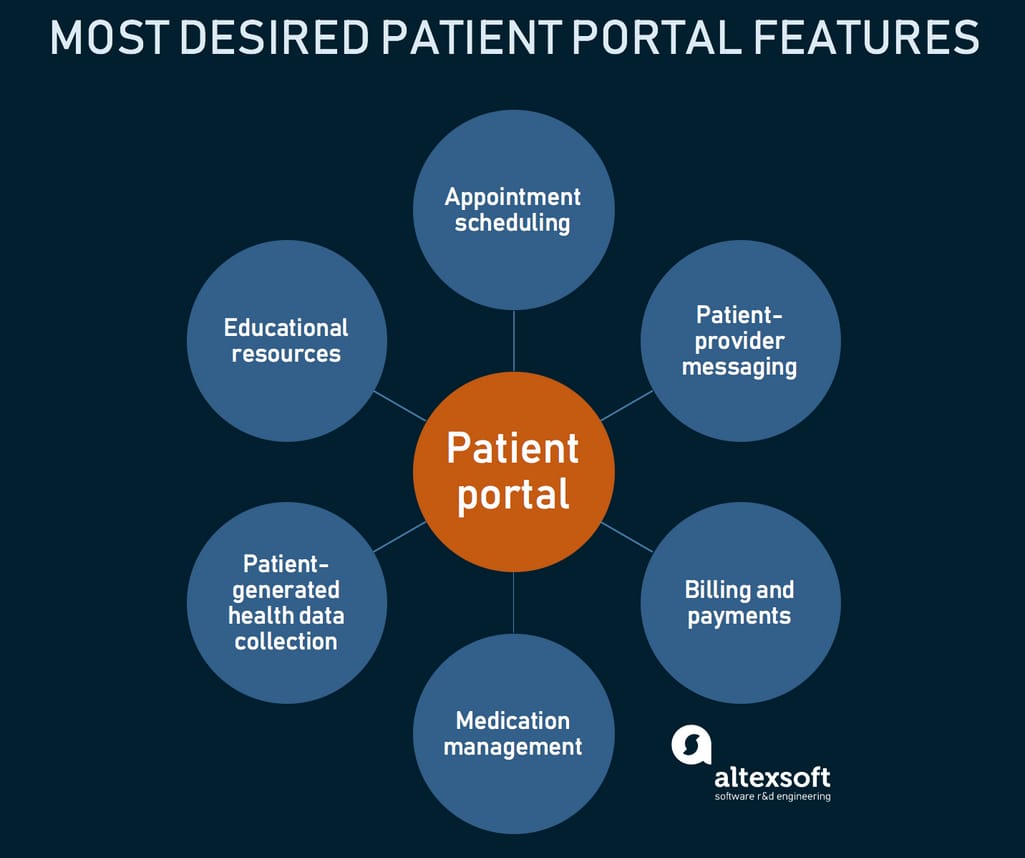
Appointment scheduling. Online scheduling is available around the clock, creates an opportunity for a patient to assess open time slots and physicians, and helps lower no-show rates. The study analyzing 134,225 visits found that online scheduling may contribute to the continuity of care. Also, since system design often requires patients to book their appointment with the doctor they’ve seen before, they end up building stronger connections with physicians. Direct booking also facilitates a large number of scheduling for general wellness checks rather than illness-related appointments.
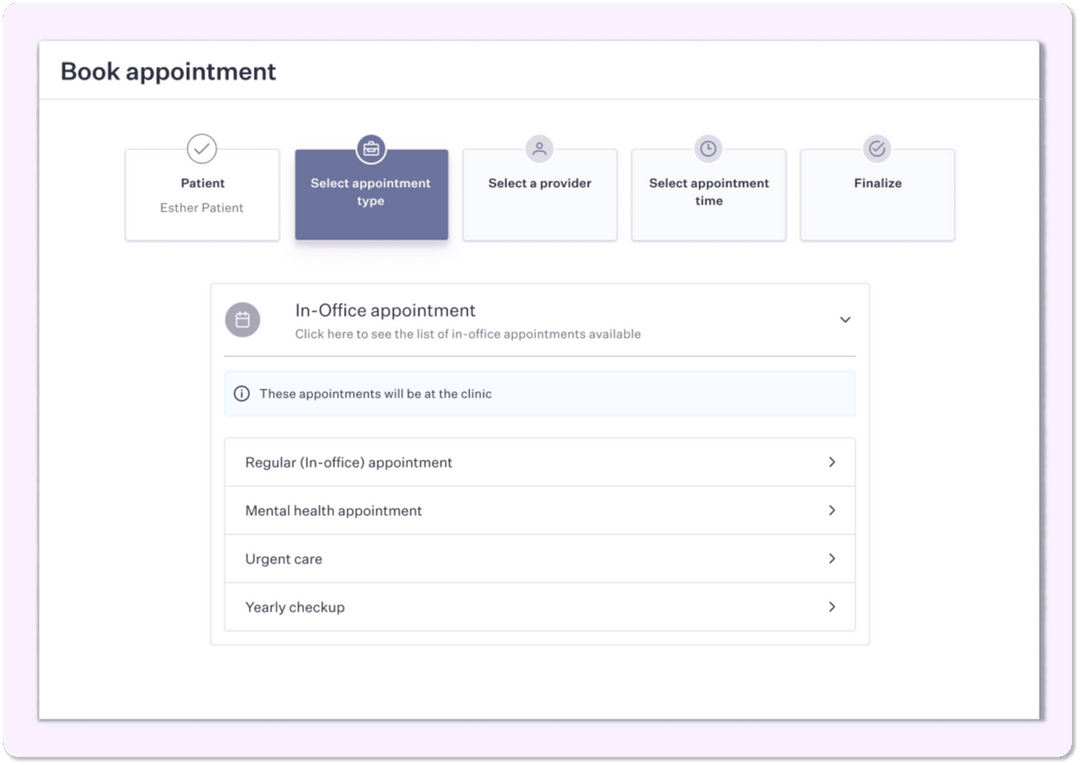 An example of a booking interface in a patient portal Source: Pomelo
An example of a booking interface in a patient portal Source: Pomelo
Secure patient-provider messaging. The use of asynchronous communication as compared to typical phone calls offers tons of benefits from avoiding missed calls, better documenting the subject of conversation, and generally making it faster and cheaper for patients to access practitioners (“this could’ve been an email”). Research shows that it also doesn’t decrease productivity of physicians, who generally don’t mind answering a few messages throughout the day.
Online billing and making payments. A patient portal is tightly coupled with your billing software. You can use the latter to send an invoice to the patient’s account in the portal, which is where patients can make secure payments. All payment functionality is provided via an integrated payment gateway, so no credit card data is stored by the clinic.
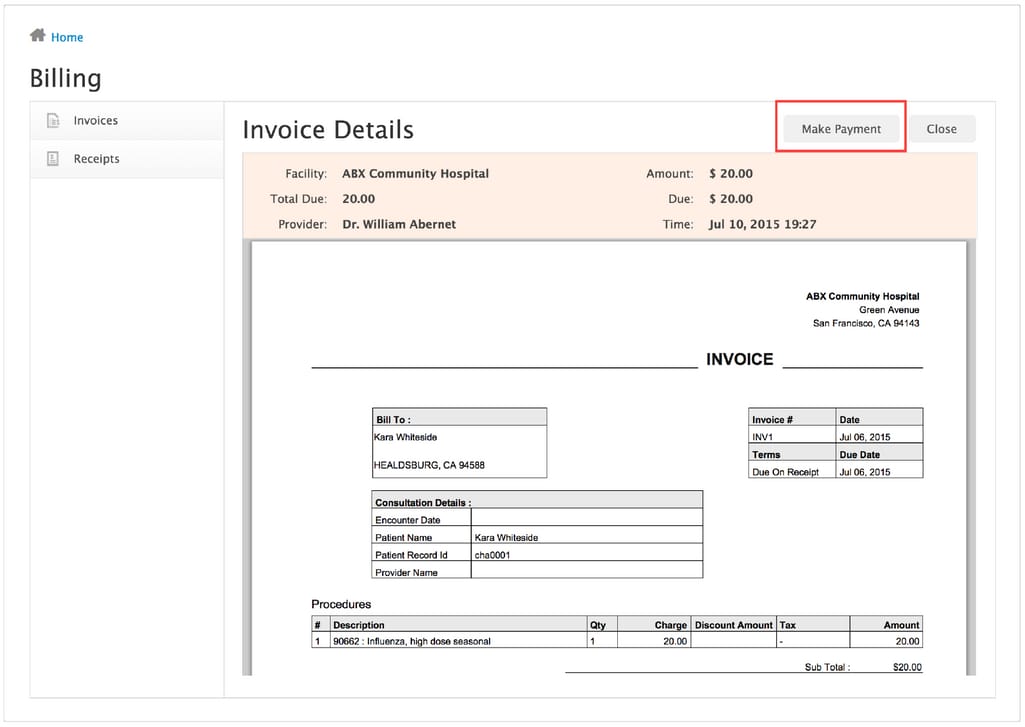 In this billing interface, a patient can access their invoices and receipts Source: ChARM Patient Portal
In this billing interface, a patient can access their invoices and receipts Source: ChARM Patient Portal
Medication management. Medication adherence is one of the critical issues that patient engagement practices are focused on. Patients have a lot to know: how long they’ll be on medication, its side effects, risks, benefits, and much more. They need help remembering why they’re even taking medication and when they should order for refills. So, this feature is responsible for two tasks: 1) displaying an updated list of their medications and dosages and 2) streamlining refills. We recommend reading our article on drug data APIs to learn what kinds of useful medication information you can provide via third-party integrations.
Ability to gather PGHD. Collecting patient-generated health data (PGHD) promises to have a clear, positive effect on a patient’s health and care. This includes data about a patient's symptoms, their lifestyle, or even biometric data from blood glucose monitoring devices and other wearables. And this is no longer an early adopter territory with 43 percent of patient portals accepting PGHD. The question is what data is accepted and how it’s used. PGHD adoption is made easier by such technologies as remote patient monitoring (RPM) tools and healthcare APIs.
RPM tools are specialized FDA-approved devices with an IT ecosystem supporting data collection, storage, and visualization. And the API technology allows patients to synchronize the apps they’re already using for data collection with the patient portal or EHR.
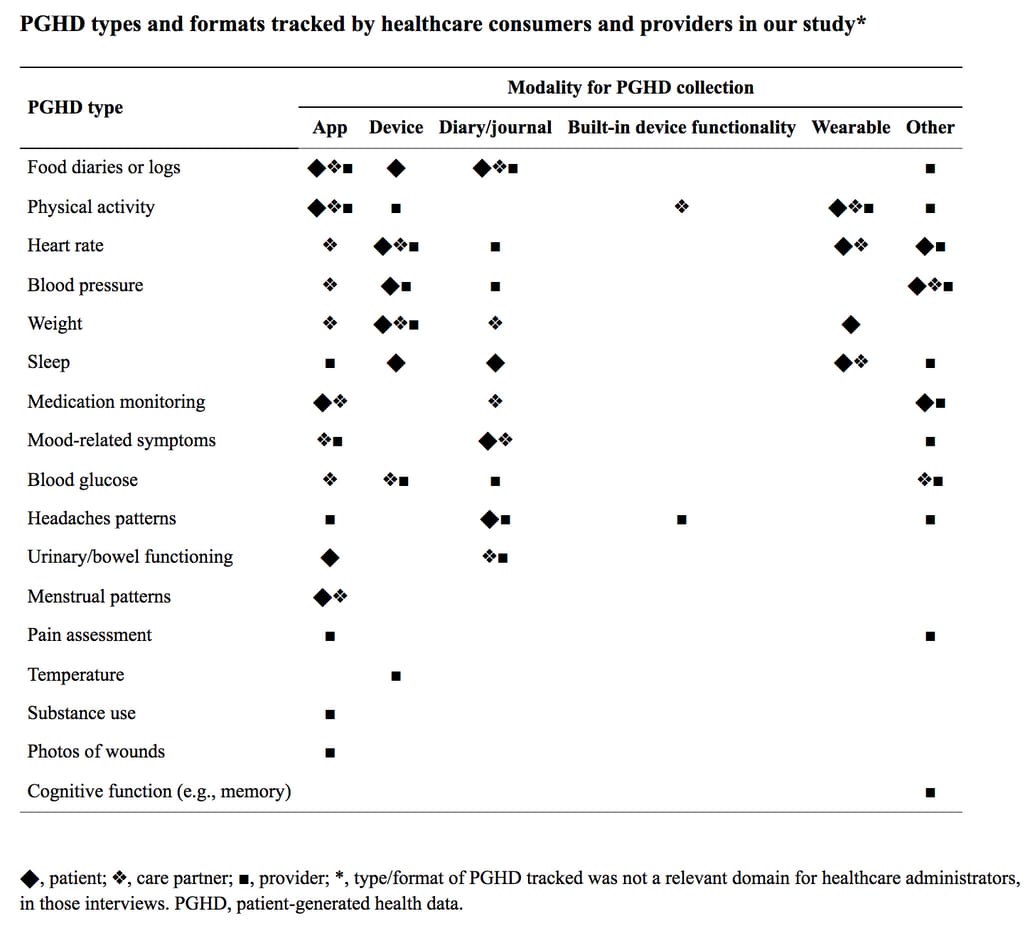 How patients and caretakers track health data outside of hospital encounters Source: mHealth and patient generated health data: stakeholder perspectives on opportunities and barriers for transforming healthcare
How patients and caretakers track health data outside of hospital encounters Source: mHealth and patient generated health data: stakeholder perspectives on opportunities and barriers for transforming healthcare
Providing personalized educational resources. Personalized educational materials like videos, spreadsheets, scientific papers, 3D models, and many more provide information to patients who wouldn’t otherwise look for it. Health literacy is especially low among patients without chronic illnesses who are not familiar with their new conditions and procedures. Your clinic doesn’t need to create those materials, though, as they are acquired through specialized vendors.
Making these features available will only be one part of work. Now, you have to make them easy to operate.
Adopt usability strategies
One of the main principles of inclusive design is to target the underprivileged and people who are not good with technology and medical terms, but the rest will benefit, too. Here are some common design practices that might help with that.
Conduct user research. One of the biggest mistakes of application development is designing with the wrong users in mind. That’s why ready-made solutions might not work for your patients. External recommendations won’t be of great use to you but talking to your patients will. So, conduct a few interviews and send out surveys to determine several user personas to outline the wants and needs of your patients.
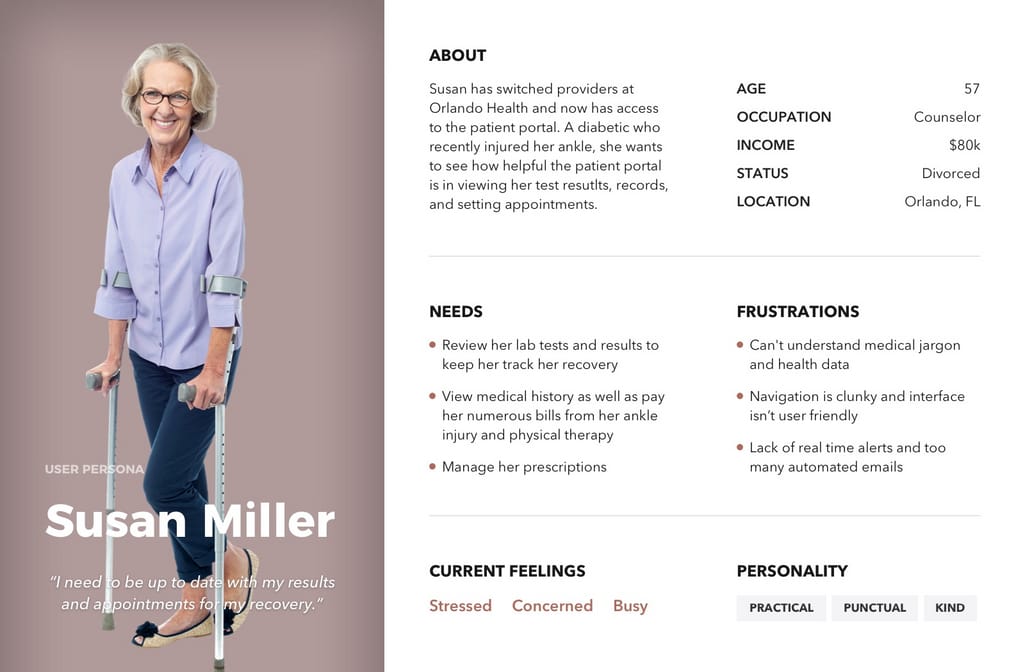 Patient persona example Source: StrongUX
Patient persona example Source: StrongUX
Consider mobile-first development. Many features a patient portal provides actually feel more natural to do on a smartphone. Messaging, booking, logging data, reviewing medication information -- all are done on the go. There are three options to deliver mobile experience:
- a mobile website,
- a progressive web app (PWA), and
- a real mobile app.
We recommend the middle choice. A PWA resides on a patient’s phone just the same as other apps, but it’s actually a link to a more polished web version of the portal. Besides, it looks and feels exactly like an app and takes much less time and money to develop.
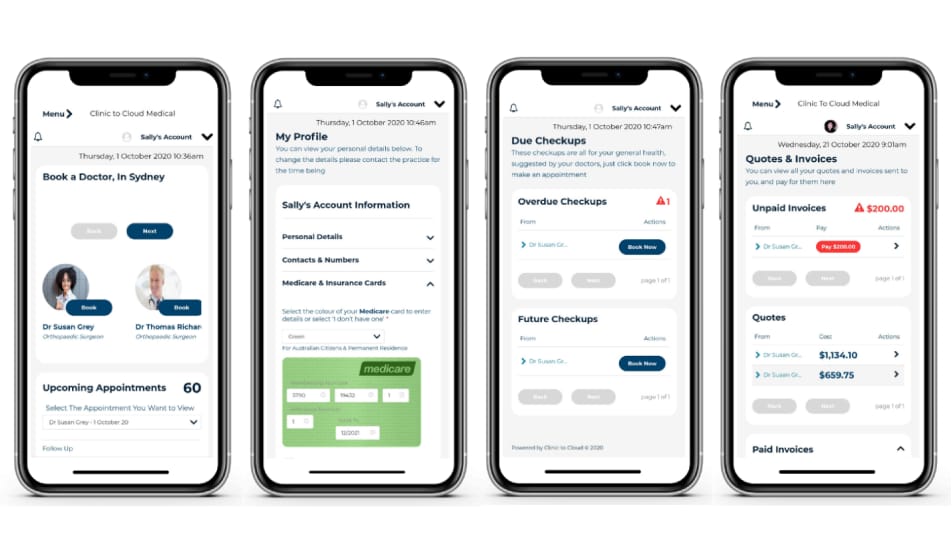 A patient portal by Clinic to Cloud Source: Healthcare IT
A patient portal by Clinic to Cloud Source: Healthcare IT
Adopt UX metrics. To test how patients react to different engagement techniques and interface features, track how their interactions change and prepare to either roll back or learn what works best.
Use relatable words and avoid jargon. Find a way to display information in a concise but clear manner. The average Medicare beneficiary reads at a fifth-grade level. So, invest in professional copywriters and UX writing experts who can transform complex medical terms and information into easy-to-understand text.
For all that, expecting people to adopt the patient portal without assistance is a bold move. Let’s see how you can educate them about the technology.
Provide portal training
One study that recorded and analyzed participants trying to complete six tasks in a patient portal, found numerous violations of Nielsen’s usability principles. People were assuming functionalities that didn’t exist, expected feedback on sent messages, and took different times to learn. Here’s how to bridge those gaps.
Incorporate an onboarding flow. Onboarding is the process of instructing new users about an application’s benefits and features. It’s commonly designed as a simple task that a user should complete in order to use the rest of the app. You can show patients how to make an appointment, locate their PHI, or message a physician. Although for a less tech-savvy user, more personal practices might be helpful.
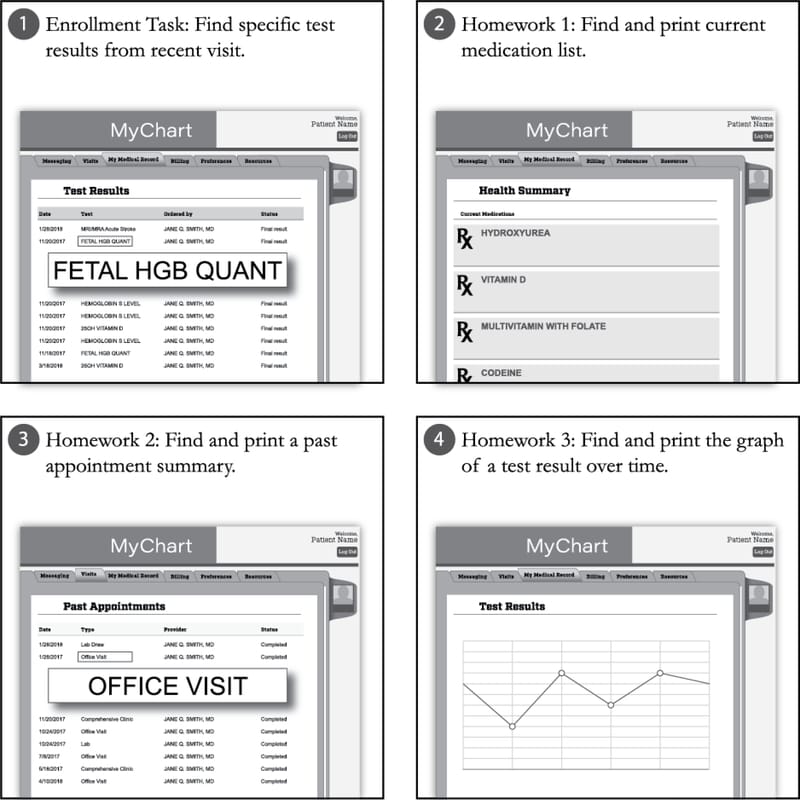 Types of mini tasks you can show patients during onboarding Source: Acceptability and Feasibility of a Disease-specific Patient Portal in Adolescents With Sickle Cell Disease
Types of mini tasks you can show patients during onboarding Source: Acceptability and Feasibility of a Disease-specific Patient Portal in Adolescents With Sickle Cell Disease
Provide in-person training. Hospital staff should be available to show a patient how to use the portal, either on their smartphone or through an onsite kiosk.
Promote the portal among patients. Patients should be aware of your portal and its capabilities. Hand out brochures, run videos on waiting room monitors, and send email links with instructions on how to register. And if they do register but don’t end up visiting the portal, follow up with a reminder.
The last practice, however, won’t yield substantial results if your practitioners are not on board. Let’s discover what they need in order to engage.
How to engage physicians
One of the main facilitators for using a patient portal is having encouragement from clinicians. Yet, there are barriers keeping practitioners from promoting portal use.
Here are some clinicians’ fears and how to address them.
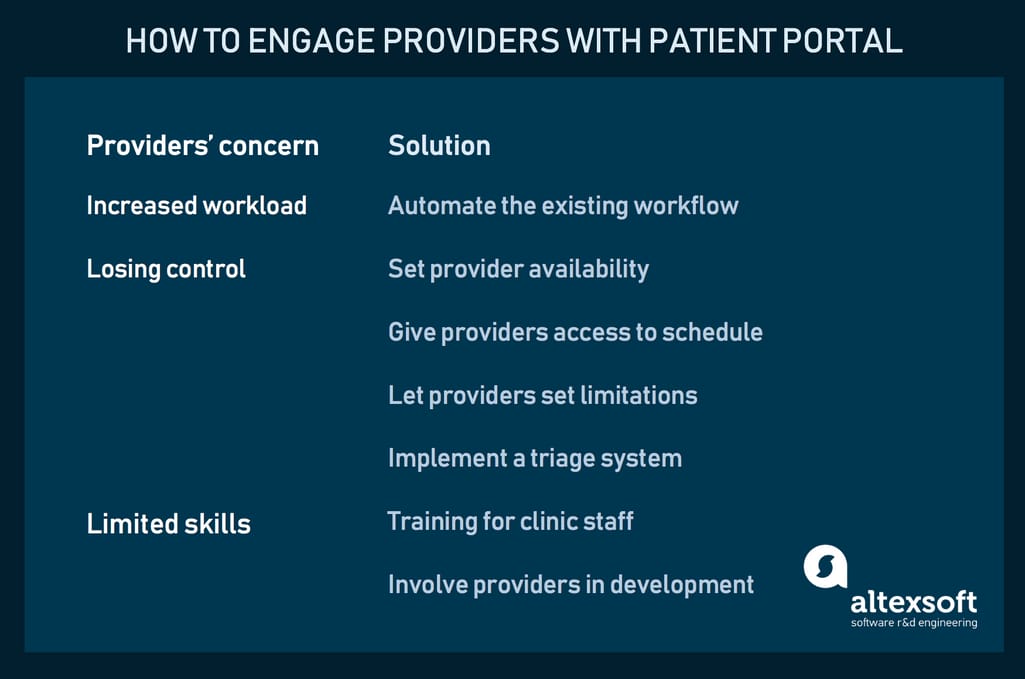 Techniques to engage physicians with a patient portal
Techniques to engage physicians with a patient portal
Fear 1. Increased workload. Although studies suggest that messaging patients hasn’t impacted workloads of primary care providers, you need to find which components of their work can be automated with a portal and present a compelling case. Some examples include: an ability to automate medication refills without having to check if the patient made a request or incorporating a template with a series of questions that helps a patient accurately describe their condition.
Fear 2. Giving control over to patients. Let physicians set the time they’re free to message, so the patient doesn’t expect a reply on the weekend. Similarly, make sure they can access their schedule and be able to change it as they would in the usual setting. Make sure they know that they’re not required to make clinical decisions based on data entered by a patient and can always initiate a formal appointment. Finally, implement a triage system, where a question can be answered by a nurse or a receptionist.
Fear 3. Having no skills to adjust to electronic interaction. While training is an obvious recommendation, another handy practice is incorporating physicians in the design process. Make clinic staff one of the stakeholders in the development project. They should be actively involved in making important decisions, sharing ideas, and testing functions. Developers and designers will be able to match their level of technical comprehension, and care providers will impact the final product.
Finally, let’s address the technical side of developing a healthcare product, specifically the one focused on PHI exchange.
How to establish data security and exchange
There are two considerations specific to health IT development: security and interoperability. Since data exchange is highly formalized in the industry, adhering to these considerations basically means adopting specific data standards.
Enable data security practices
In the US, PHI is protected under HIPAA Privacy and Security Rules. (GDPR performs the same function in the EU.) Under HIPAA, healthcare providers must enable cybersecurity measures. In practice this means such procedures as:
- Authentication -- managing a patient's identity using such methods as a username and password, a “knowledge” question, email verification, and multi-factor authentication.
- Automatic log out after a period of inactivity.
- Secure storing of data on a user’s device and its deletion on logout.
- Regular technical vulnerability assessments.
- Explaining data breach risk to patients.
One of the most difficult tasks is hitting the right balance between security measures and ease of use.
Adopt data exchange standards
Under the Interoperability Final Rules, all healthcare providers must implement two data exchange standards: FHIR and USCDI. They take care of seamless communication between different healthcare systems, including EHRs and patient portals. Apart from this compliance minimum, there are standards for other data exchange purposes:
- Direct that handles safe patient-provider message exchange.
- DICOM that defines how and in what format to transport medical images.
- SCRIPT that relates to exchanging electronic prescriptions between providers, pharmacies, and health plans.
- CDISC that defines how clinical research data should travel.
One of the biggest opportunities in data exchange implementation is providing health information exchange (HIE) -- the ability to share data between different providers, rather than just within one clinic. For example, instead of going to one portal and printing their medication list to show their doctor in a different clinic, patients should be able to simply share the list with a different account. There are several approaches to facilitate such exchange between portals.
Directed exchange. Clinics that trust each other easily and securely send laboratory results, discharge summaries, medication lists, and more via the Direct standard.
Query-based exchange. Physicians search for accessible sources on a patient, for example, in an emergency room, via an integration with one of many health information networks such as CommonWell and the eHealth Exchange.
Consumer-mediated exchange. Here, patients coordinate their data similar to how they manage their finances in online banking. They use the same interoperability technology as in internal communication and the only thing needed is the open API from another provider.
The business case for patient portals
Unfortunately, there’s no documented evidence that the use of portals results in cost savings and operational efficiencies. Though some vendors claim financial benefits, it’s no guarantee that the same will happen with your clinic. The benefit is more indirect.
For example, patients with portal accounts are more loyal to their provider and are more likely to return. Higher retention rates translate to higher revenue. That is, of course, if the portal offers some real benefits.
Another point is that when your practice grows, you don’t need to hire more admin staff as the portal scales almost indefinitely.
Besides, you can always start small. Work with your development partner to recognize the patients’ most pressing needs and meet them first, for example, by integrating messaging and scheduling capabilities via available APIs. Test, iterate, and work your way up as you see results.

Maryna is a passionate writer with a talent for simplifying complex topics for readers of all backgrounds. With 7 years of experience writing about travel technology, she is well-versed in the field. Outside of her professional writing, she enjoys reading, video games, and fashion.
Want to write an article for our blog? Read our requirements and guidelines to become a contributor.

