Today even doctors can be shipped right to your computer. While remote patient care and online appointments are nothing new, the Telehealth and Telemedicine concepts became a hot topic thanks to the COVID-19 pandemic.
As announced by Medicare and Medicaid, the number of individuals accessing telehealth through the Medicare system has increased from 11,000 to nearly 650,000 people a week. In the US, regulations concerning telehealth were temporarily relaxed. In contrast, European countries like France passed legislation regarding telemedicine and teleradiology back in 2009.
But that said, numbers and dry facts don’t reflect the real state of telehealth adoption. As the HIMMS 2019 eHealth report claims, telemedicine adoption is the second biggest trend among healthcare organizations in Europe. So, this article explains telehealth and telemedicine concepts. We’ll give you an overview of the technologies existing and discuss the adoption blockers and opportunities for healthcare organizations.
What are telehealth and telemedicine?
Let’s define terms and start out with some textbook explanations.
Telemedicine is the practice of using communication technologies (chats, phone/online calls, video conferences) to connect doctors at one location with the patient at another. The apps used for appointments, examinations, and imaging transcripts present an alternative to in-person meetings. This helps doctors and patients to be safe in the case of pandemic conditions and/or increase the reach of medical services for distant areas.
Telehealth is a broader term that specifies the use of communication technologies both for clinical and nonclinical services. Nonclinical services include training staff, information distribution, hospital management conferences, etc.
In reality, the terms are often used interchangeably, as telehealth comprises telemedicine and other technologies improving clinical and administrative operations via telecommunication. Telemedicine is now in great demand in healthcare organizations. McKinsey says that not only does the interest in virtual medicine grow in medical facilities, but also among patients. So it seems, even after COVID-19, telemedicine will remain a way to bring doctors and patients together because of its convenience.
So, now let’s have a look at the actual capabilities of telemedicine and the technologies that support it.
Telemedicine practices and technologies
Telemedicine is a multipurpose practice that extends medical services both for critical and noncritical circumstances. Generally, it’s used to treat patients that are out of reach, unable to come in person, people who are immobile, bedridden, or have chronic diseases. On the other hand, a facility lacking an available ambulance crew or other staff can compensate with the help of telemedicine.
Noncritical occasions include treatment of patients with mild illnesses, sharing data investigation details, or imaging results. Patients can also purchase medications and receive prescriptions via a dedicated application or web portals.
So, what are the practical use cases and what technologies are used for it? Shashi Gogia’s book The Fundamentals of Telemedicine and Telehealth suggests 4 methods of providing telemedicine.
- Real time communication
- Store and forward
- Telemonitoring or remote patient care
- Mobile health
Let’s take a look at each of them in detail.
Real time communication
Real time communication makes use of any communication technologies to contact the patient. Video conferences, live chats, voice messages, and emails are the primary examples here.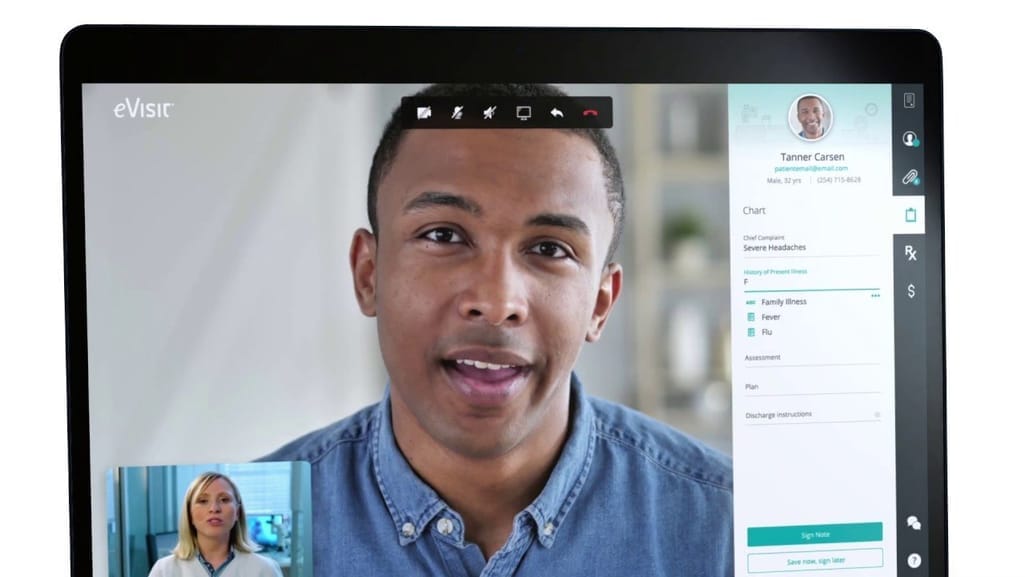
EVisit video conference application
Source: evisit.com
Since clinical data always has to be secure, tools like Skype or Messenger are rarely used as an official method of communication. Such tools are often available as a built-in application on telemedicine platforms, e.g., Intelligent Medical Software or eVisit. These systems are often integrated with internal healthcare systems and guarantee compliance with existing data privacy policies.
The real time data exchange is also called synchronous, as we analyze and transfer information right away. And these telemedicine applications are often integrated with each other. So, it gives patients and doctors easy access to connect through a single app both to communicate and to share data.
Store and Forward
Store and forward entails collecting direct patient data and forwarding it to the corresponding specialist. This data can be a recording of an appointment or a test result, which is placed in a single file to be stored in a database of an Electronic Health Record (EHR) system.
Since this practice helps doctors analyze the data afterwards, it is called asynchronous communication. Synchronous and asynchronous communication techniques are often used in conjunction.
The flow of data between clinical IT components may differ but the sense of it is to make the recordings available for editing, commenting, and sharing between the doctors. Healthcare analytics are often a part of such systems as they can work with the collected data and access it via a user interface. So, in the long run, store and forward methods suggest better time and resource management but can delay the results and treatment.
Telemonitoring or remote patient monitoring
Remote patient monitoring or RPM is a practice within telemedicine aimed at monitoring the vital statistics of the patients remotely. Telemonitoring relies on different electronic devices that stream patients' statistics right to a healthcare provider's analytical interface of. For example:
- Ultrasound imaging. Phillips introduced a smart device called Lumify, portable gear used to transfer ultrasonic sound information from a patient to a doctor. The device is connected to a tablet or a smartphone via cables, basically allowing the patient to perform ultrasound examination and broadcast it to the healthcare provider.
- Tele-stethoscopes. There are various products on the market like Digital Stethoscope by AMD Global Telemedicine. Basically, it's an electronic stethoscope connected to a laptop that transfers high quality heart or lung sounds via a dedicated portal. This way, healthcare providers can analyze the state of a patient, receive precise data about symptomatology, store the test results, and use them in the future.
Digital stethoscope data transferred to a clinicians app
Source: amdtelemedicine.com
Mobile apps are used as a connector between the device and a hospital’s internal system. This system consists of a database and interface. Dedicated modules can send alerts, analysis reports, and support clinical decisions with the data and visualizations.
These systems are used to care for patients with chronic and critical illnesses using remote monitoring. Children’s Health hospital was one of the first to use RPM to monitor patients during the postsurgical period. Using Vivify RPM platform and tablets, the doctors monitor patients and conduct virtual visits, a successful use of telemonitoring.
Mobile health or mHealth
Mobile health applications are widely used to support telemedicine. Generally, mobile applications connect an electronic clinical device with software. But they can also act as a standalone tool.
For example, Welldoc’s Diabetes Manager is capable of using input data of food a patient consumed and calculating blood-glucose information based on it. Also, the patient is provided with a personalized health coach that gives prescriptions and recommendations for diabetics.
Mobile MIM is a specialized app for sharing cardiology, radiology, oncology imaging as well as other types with physicians. The app allows patients to pass screening results and communicate with the healthcare provider.
Mobile teleradiology
Source: mimsoftware.com
The ease of distributing mobile applications on the AppStore and Play Market makes mHealth a fast-growing technology. Using mobile apps for various tasks, a hospital can optimize the use of a its space, speed up communication, share more data, and conduct some clinical procedures remotely.
Telemedicine use cases
The practical use cases of telemedicine are numerous. Almost every healthcare branch has a handful of application scenarios. To give you a brief overlook at use cases, we provide a short list of examples, which is by no means exhaustive, but will give you with a general idea:
Dermatology. Sharing photos of skin pigments, nevii, scars, rashes, or abscesses for immediate consultation.
Cardiology. Monitoring patients with cardiac diseases via wearables or examination using electronic stethoscopes and tele-ECG.
Ophthalmology. Macro photography of an eye with the help of smartphone camera and optical attachments.
Psychiatry. Video consultation and prescriptions via mobile apps.
Emergency care. Providing instructions and consultation while waiting for emergency support.
Orthopedics. X-ray image sharing, monitoring, and consultation.
Nursing. Nursing services for noncritical cases and minor injuries, like bruises and mild burns. Instructing on wound treatment and medication.
Physical therapy. Guiding patients on sport or other injury treatment by prescribing different exercises, diets, and regimes.
The benefits of telemedicine
So, as you can see, telemedicine technologies cover a wide range of cases. Each case brings its own benefits that improve overall operability for the hospital. Let’s quickly summarize them here.
Reduced or no transportation time/cost. In some cases, in-person visits are inevitable. However, telemedicine enables healthcare providers to make observation at any time for numerous patients without leaving the hospital. So, the transportation costs both for clinicians and patients are drastically reduced.
Improved scheduling. With the help of online appointments, half of the waiting lines move to the internet. This saves a physician’s time spent on appointments and makes scheduling more precise.
Optimized hospital space use. Allowing appointments and monitoring via telemedicine also helps to unburden emergency rooms and take care of patients in a more critical state and also cut costs.
Reduced contagion risk. Hyper valid for the pandemic time: the less people visit in person, the less risk of infection for everyone.
Access to a wider pool of specialists. As we noted, smaller hospitals may not have a specialist or department in-house. With the help of telemedicine, hospitals can share patient data with each other and provide treatment much faster.
Constant monitoring. Providing care for patients that require monitoring helps to reduce general health risk. Additionally, it’s also way to cut emergency room visits and the cost of the care.
The challenges of telemedicine adoption
Benefits can serve as a basis to initiate the adoption of telemedicine practices in your healthcare organization. However, individual hospitals and industry as a whole are facing certain challenges that inhibit the development process. These are the major ones.
Reimbursement coverage and regulations
Especially in the US, regulations concerning telemedicine are quite harsh and tangled. Government payers Medicare and Medicaid set the rules for service reimbursement. These policies regulate telemedicine reimbursement for every type of service (real time, store and forward, etc.).
So, the maze begins with the reimbursement coverage and its details, e.g., Medicare provides reimbursement only for video calls made of non-metropolitan (rural) areas, or Health Professional Shortage Areas. Meaning that patients living in big cities can’t call from their homes.
For now, there is also no law requiring private payers to reimburse telemedicine services like the regular clinical ones. This caused a development of a parity law, which equates the rules and rates of reimbursement for telemedicine and regular services. But this law is currently active in seven states, while regulations still differ from payer to payer.
As we mentioned at the beginning of the article, this year the regulations were relaxed: Cigna, UnitedHealthcare, and Humana temporarily changed their reimbursement policies for a number of telehealth services or billing mechanics. But whether these changes will become permanent is unknown.
To learn about policies in your state, visit the Center for Connected Health Policy website or view their 2020 report on telehealth reimbursement policies.
Data privacy and interoperability rules compliance
Telemedicine utilizes a lot of personal patient data. As we’re talking about collecting, storing, and transmitting the information, we also need to take into account specific requirements in this field.
HIPAA is a data protection regulation that governs patient data transferred both via telemedicine technologies and internal clinical systems. You can learn more about the most common HIPAA violations in our dedicated article.
GDPR, as a general data protection law in Europe, is valid for all the internet technologies working with personal client data.
CCPA is the data privacy law for the state of California.
PIPEDA deals with personal information protection and electronic document exchange policy for Canada.
Data Protection Act 2018 determines how personal information is used in the UK.
From November 2020, new interoperability regulations also became effective. These standards describe how data exchange should be held and which data should be exposed to the patient. The end goal of those interoperability changes is to establish unified data exchange rules in healthcare and enable “shopping” medical services on devices.
FHIR determines the way the data is exchanged using RESTful APIs to exchange data in healthcare applications. The files can be written in one of three formats: XML, JSON, and RDF.
USCDI regulates the relationship of the healthcare organization and the patient.
You may read our article on how to comply with interoperability requirements in healthcare.
EHR integration
The electronic health record (EHR) system is the heart of healthcare IT infrastructure. While EHR doesn’t store treatment history, it is a central system other components integrate with. That means telemedicine is also integrated with EHR.
The problems with EHR is described by The Office of the National Coordinator for Health Information Technology as 4 general issues.
- Capturing clinical documentation applies its own requirements that follow up with tons of “fill-in” work.
- Most EHR systems are poorly designed in terms of user experience and convenience.
- EHR reporting imposes another burden as the reporting requirements for the EHR systems are often misaligned with federal programs.
- There is a lack of interoperability between state prescription drug monitoring programs and EHR.
These challenges make integration with EHR difficult. It’s hard to follow all the required standards for data exchange. In the case of RPM or real time communication, lots of data is constantly generated. The existing EHR policies are counterproductive as compared to the logic of quick data transmission and access as it requires clinicians to fill out unnecessary documentation and deal with bureaucracy.
So, to avoid integration issues and lags in dataflow, start with EHR. The topic of complying with aforementioned requirements is very broad. We’ve previously provided concise guidelines on how to fix EHR problems.
Accessibility
According to the Federal Communication Commission, 6 percent of the US population doesn’t have constant connection to high speed internet. That’s over 19 million people with nearly 14 million living in rural areas.
As telemedicine primarily focuses on out-of-reach patients, the lack of internet connection in remote areas only aggravates the problem, as healthcare providers won’t be able to transmit data. On top of that, this prevents streaming data from wearable devices used for telemonitoring. But the problem doesn’t have a solution in sight since broadband coverage develops over years.
Training burden
Any technology requires both clinicians and patients receive proper training on how to use it. Telemedicine devices and applications are no exception. This burden falls on the healthcare provider, as they will need to establish training and information broadcast for different groups of users, involving additional costs, excluding the telemedicine platform itself.
While patient applications are prone to be user-friendly, the internal systems may consist of numerous analytical interfaces. The best way to address this issue is to rely on IT healthcare providers to formulate guidelines and design training methods. A great deal rests on the UX of the developed platform to eliminate a major part of the training burden.
How to initiate the telemedicine adoption process?
Taking into account the existing challenges and benefits of telemedicine technologies, there is still a big demand on remote care and monitoring. So, to help with making the decision, here’s a six-step guide to address the major strategic points.
Step 1. Define the goals
Telemedicine application and the range of services included in remote care depends on the problems a healthcare organization is trying to solve and the desired goals. Some of the common goals may be
- increased healthcare facility revenue,
- reduced hospital readmission,
- widened accessibility of the healthcare services,
- optimized hospital space utilization, and
- decreased load on the ambulance crews.
This will help identify the required applications and practices to adopt and invest in.
Step 2. Develop a use case
As we mentioned before, telemedicine is designed for specific use cases. To run the discussion with your internal and external stakeholders, develop and document a use case for the telemedicine technology.
Let’s say the major group of your patients are seniors suffering from chronic respiratory or cardiac disease. In most cases, such patients require constant monitoring to prevent risk situations and complications. Telemedicine resolves the issue by providing both hardware and software to monitor patient health at home. This can be a use case for a cardiovascular or nonspecialized healthcare organization.
Step 3. Gather requirements
After you define the target audience and develop a use case for a telemedicine tool, it’s time to have a discussion with staff and stakeholders. This step can be considered as requirement gathering: Input from your clinicians will give you a better understanding of what type of tool is needed, who will use it, and how. Additionally, this will reveal more details on your healthcare data and process flow so you can understand how a new technology can be integrated into the existing infrastructure.
For the majority of hospitals, EHR systems are the main technology to integrate with. So, you’ll need to analyze the possibilities of integration with your specific tool and calculate the budget for the initiative.
Step 4. Research the market
Exploring a single article on telemedicine capabilities provides only general understanding of a topic. You will need to research more of the existing solutions and look at the providers’ conditions. Here, we’ll cover some examples of the existing platforms to show the diversity of the market.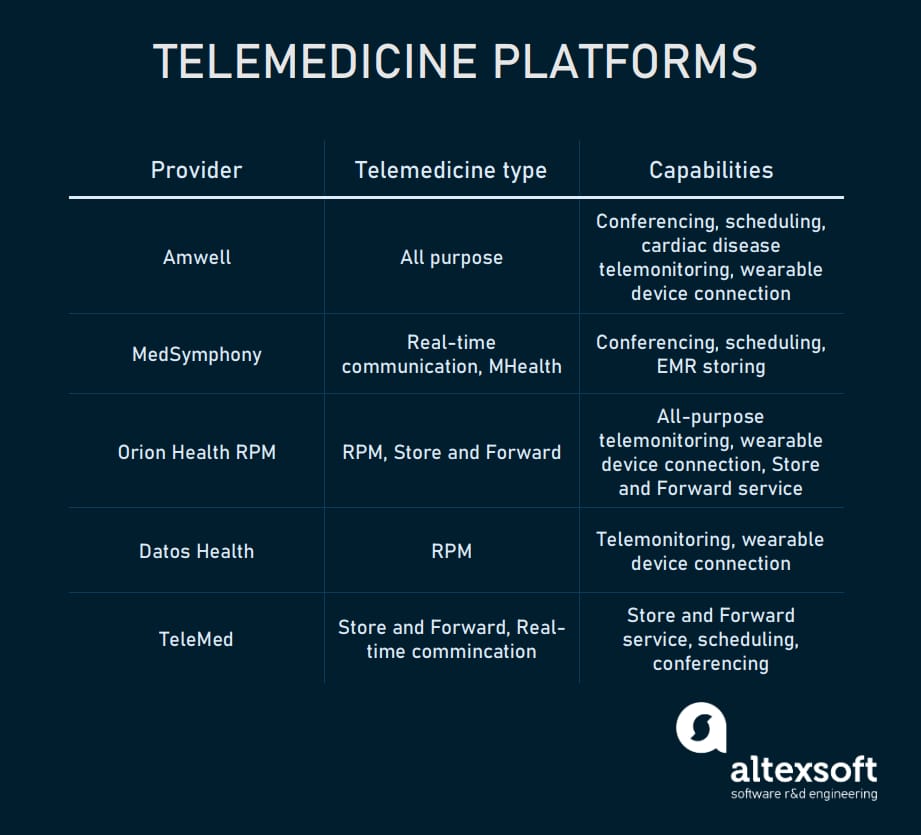
Telemedicine platform providers
Amwell is one of the largest telemedicine platforms and contracts with Anthem insurance company. Available modules: real time video conferences, physical and psychiatric treatment, urgent care, and telemonitoring for cardiac disease.
MedSymphony is a video conferencing platform that tracks and manages EMR via a mobile portal, which can be considered an mHealth platform.
Orion Health RPM is a platform for telemonitoring and store and forward telemedicine. Orion RPM provides software to collect and register patient activities, send prescriptions, and monitor their daily routine. Wearables are responsible for streaming vital signs data.
Datos Health is an RPM platform that consists of a patient mobile app and a dedicated analytical cloud service for clinicians. Datos connects with various wearables to source the data, pass it to the interface, detect abnormalities, and send alerts.
TeleMed is a platform that includes 4 separate modules: a scheduler, virtual waiting room, medication kiosk app, and store and forward service. The latter service is mainly designed for dermatologists and radiologists to collect data and pass it to the practice group that writes prescriptions.
Step 5. Check the integration capabilities
Some providers, like Amwell, offer out-of-the-box integration solutions for the most popular EHR systems, like Epic, Cerner, or Allscripts. If you're using a less popular system, there might be some issues with integration and interoperability between the tools.
Check interoperability and integration options with providers directly. There also may be the need to set up custom integration between telemedicine and the rest of the technology ecosystem.
Step 6. Consider a custom tool
For the most part, the telemedicine market is dominated by video-conferencing platforms that offer data privacy, scheduling of appointments, and payment mechanisms. But there are just a few combining remote care and real-time communication capabilities. Or the RPM part can be designed for one clinical specialization but not for others.
The solution here is to design custom software for your healthcare organization. Of course it depends on the specific use case, but generally, managed systems don’t cover the whole variety of treatment opportunities suggested by telemedicine. Eventually, you may either need customization from the vendors or building a number of systems from scratch based on the specific facility requirements so it covers missing functionality.
The market is still forming as telemedicine is a relatively young field both for healthcare organizations and software developers. And that’s why a custom platform may be the wisest choice.


